I am an IBCLC (International Board Certified Lactation Consultant) in private practice in Northern Ireland and a La Leche League Leader with La Leche League of Ireland
Experiences of Tongue Tie Treatment in Northern Ireland

As an IBCLC (International Board Certified Lactation Consultant), I work a lot with tongue tie or anklyglossia and deal with many families who come to see me because they suspect a tongue tie. I may be educating families about tongue tie, working through complex breastfeeding issues that aren't resolving through basic support, assessing a baby's tongue movement during a consultation, referring babies to a surgeon / tongue tie clinic, or helping with breastfeeding after the tongue tie has been released. More and more however I find that I am being contacted by parents who have already had a tongue tie released, but their experience has been that the release has not resolved their problems. Also more and more I hear that these babies have been referred "just in case" there is a tongue tie, or because "there may be a slight tie". I have also heard from parents who tell me their baby's "tie " was snipped even though they were having no breastfeeding difficulties, breastfeeding was comfortable, baby was content and gaining well. All of this concerns me in how tongue tie is being assessed, treated and followed up, so I decided to try to get some feedback from parents about their experiences of tongue tie treatment in Northern Ireland.
Before we go into the experiences it's important to state that tongue-tie (anklyglossia) is a condition which can cause enormous problems for breastfeeding, and even for bottle feeding and eating solids for some babies. It affects somewhere in the region of 3-10% of babies (most studies put it at around 3-5%), and has a genetic basis so we often see it run in families. A tongue tie occurs when there is an abnormal frenulum (piece of issue below the tongue) which prevents the tongue from moving properly. A frenulum is NOT a tongue tie. A frenulum is normal and almost all of us have a frenulum, and its job is to stabilise the tongue. A tongue tie only exists if the frenulum is abnormal, and that can only be determined by an assessment to see how the tongue moves rather than just looking at whether a frenulum is present. Without a correct assessment a normal frenulum can be misdiagnosed as a tie. Please see my earlier blog on the difference between a normal frenulum and a tongue tie, and the kind of assessment needed.
In Northern Ireland we have approximately 25000 babies born each year. Around 50% of those begin breastfeeding - so around 12500 babies. Currently NICE guidance is only available to treat tongue tie in babies who are breastfeeding, so we might expect somewhere in the region of 375 - 1250 of those babies to have a tongue tie. It is my understanding that over 3000 babies a year are currently being treated. If anyone can get me exact figures on this, I'd love to see them.
Two weeks ago (August 2018) I created a survey to ask parents for their experiences of tongue tie assessment and treatment in Northern Ireland in the last 2 years. I collected 295 responses, and this is a summary of the data. I present a summary of the data below with some explanation of what is happening in practice.
The Survey
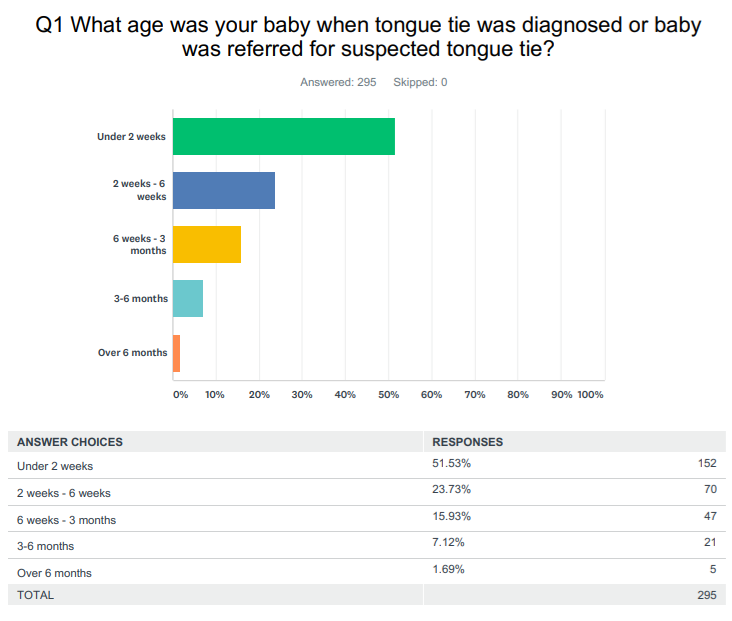
QI - When was the baby referred or diagnosed? Diagnosis of a tongue tie can only medically be given by the surgeon / practitioner who performs tongue tie release procedures (frenotomy), so although a midwife / HV / IBCLC may be able to assess, to state that tongue movement is restricted and to refer for a procedure, they cannot actually diagnose. This is why the question states referral / diagnosis separately. In NI the length of time between referral and seeing the tongue tie clinic should only be a few days. Two tongue tie specific clinics currently exists, one within the Northern Trust, situated within Antrim Hospital, and one in a Belfast clinic serving the rest of the trust areas. I am aware that a very small number of people are referred through ENT and this is often a much longer process due to waiting lists. A smaller number again, may see an ENT surgeon privately through private hospitals. The vast majority of babies are currently referred in the first 2 weeks (over 50%).
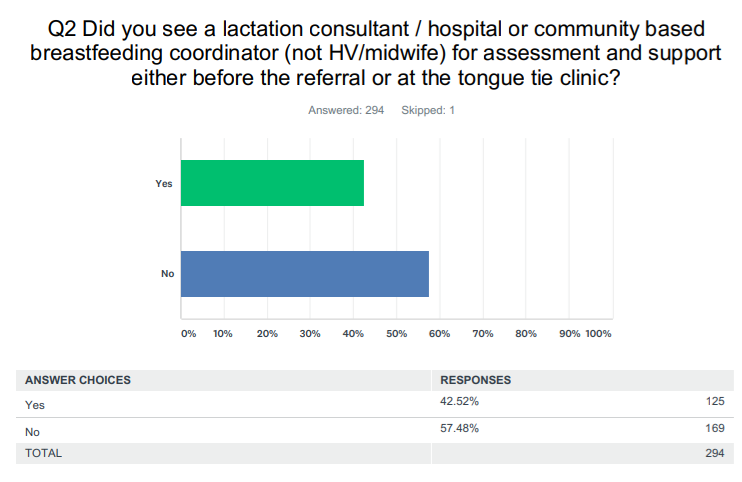
Q2 - Did you see a lactation consultant or breastfeeding specialist for assessment and support? NICE guidance on ankylglossia states that "breastfeeding is a complex interaction between mother and child, and that many factors can affect the ability to feed. Skilled breastfeeding support is an integral part of the management of breastfeeding difficulties."
HVs and midwives do not have the same training in resolving breastfeeding difficulties or in tongue tie assessment as a specialist, such as a community based IBCLC or hospital breastfeeding coordinator, and a referral pathway exists to specialists if issues are not resolving through basic breastfeeding support. Private IBCLCs are also available in the community.
The survey results showed that almost 60% of breastfeeding dyads were not seen by a breastfeeding specialist.
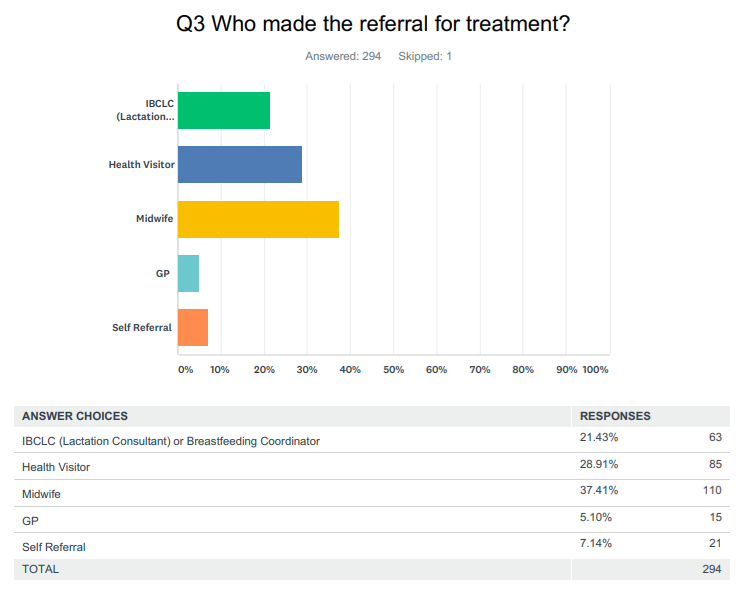
Q3 - Who made the referral for treatment? Referrals can be made to most NHS tongue tie clinics by a midwife, HV, GP or an IBCLC. Referrals through ENT generally come from HV/ GP or midwife. Some surgeons also offer a private service and parents may choose to self refer to a private surgeon.
The survey showed a mixed result for this. The majority (almost 40%) came from a midwife. This ties in with the fact that most babies were referred in the first 2 weeks, as women generally continue to be under the care of community midwives for the first 10 days postpartum. A further almost 30% are referred by a HV (who usually takes over care at around 10 days). The figures I find most interesting here are the fact that 42% of babies see a lactation consultant /breastfeeding specialist but only half of those babies are actually referred by a lactation consultant/breastfeeding specialist. I see 2 possible causes for this - but am interested in feedback for any different reasons. The 2 causes for this that jump to mind are: 1) that the lactation consultant / breastfeeding specialist who saw the baby did not believe there was a tongue tie or a need to refer; or 2) the baby was seen at the tongue tie clinic by a lactation consultant / breastfeeding specialist. This 2nd option is undoubtedly the case at the Antrim clinic where an IBCLC undertakes the procedure, but I'm not aware of breastfeeding support at any other clinic locally.
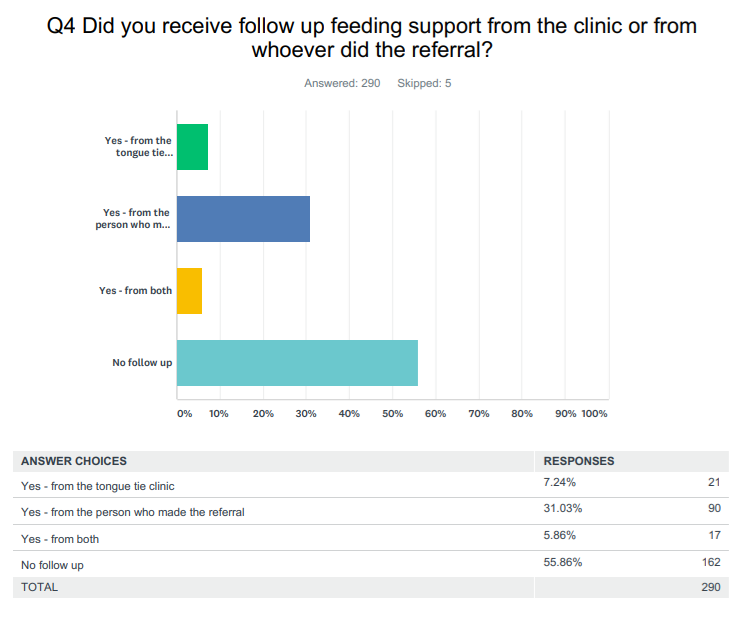
Q4 - Did you receive follow-up feeding support? The NICE guidance for treatment of ankyloglossia emphasises the importance of support by referring to a study which found that 95% (19/20) of babies who had support from a lactation consultant had improved breastfeeding 48 hours after tongue- tie division, compared with 5% (1/20) of babies in the control group (p < 0.001). (Hogan 2005). In the survey I suggested that this support may come from either the clinic or the person who referred, and I did this because there are very different services offered in different clinics. Best practice would be that a surgeon /practitioner either has breastfeeding support experience or works with an IBCLC/breastfeeding specialist to provide this. This follow up may be different in different clinics. With regards to breastfeeding - for those who were given good support before hand, given clear expectations and a plan to work on after the procedure, it is likely that something like a phone call to re-iterate the plan and check progress against it may be enough. For others it may require more intensive in person support. From a medical/surgical perspective the surgeon/practitioner may want to follow up for his/her own information on the results of the procedure.
The survey found that disappointingly almost 60% of people felt that they had no follow up feeding support whatsoever. It may be that there is a gap here that people are falling through. It may be that some HVs/midwives/GPs who refer believe that there will be breastfeeding support and follow up provided at the clinic in the same way that if you refer to physio or orthopaedics for example, that team takes over the care. In practice however, it is my understanding that only the Antrim clinic has staff trained in breastfeeding, and the other clinics are essentially surgical clinics only.
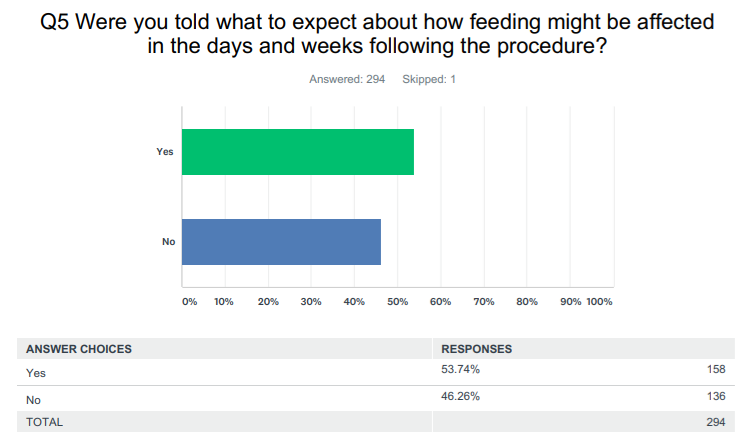
Q5 - Were you told how feeding might be affected by the procedure - essentially I was asking about expectations going into the procedure. A tongue tie release can often be presented as an instant "fix" to breastfeeding problems, however in my experience this is not the case in practice. In reality for most
babies there are still issues to work through, and feeding may actually get worse temporarily. Understanding what typically results from the release is vital to setting expectations. There are also many variations of anatomy and some babies are likely to have better results than others from the procedures, and this is important to discuss also.
The survey found that experiences were almost 50/50 with only 54% having been told how the surgery would affect feeding, and 46% who were not told. This seems quite surprising given the the surgery is presumably being undertaken due to feeding difficulties?
Some of the comments showed that quite unrealistic expectations had been set or that nothing was discussed:
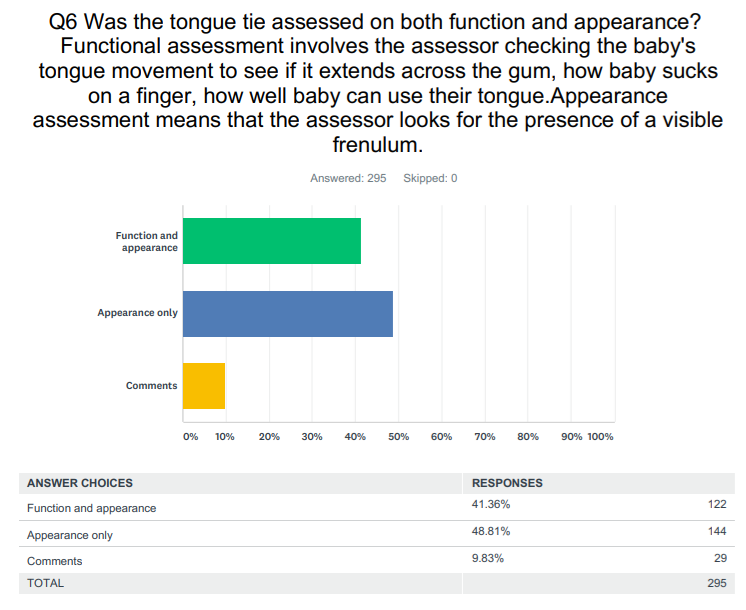
Q6 - Was the tongue assessed by function and appearance (best practice) or appearance only. Again the difference is dealt with in details in this previous blog on a tongue tie versus a tongue frenulum.
Research suggests that we can only accurately assess using both function and appearance as this is the only way to tell whether a frenulum is normal or abnormal. Without this functional assessment we risk carrying out procedures on babies who do not need them.
41% of people felt that their baby's tongue was assessed by function and appearance (best practice). The larger number (almost 50%) however felt that it was assessed on appearance only. 9% may have been unsure and chose to comment instead. These comments suggested that the parents felt that no real assessment had been done, or they felt unsure of what kind of assessment had been done, e.g.
"Unsure how assessment was done ... a finger in the mouth I think"
"Appearance only but could see that the tongue didn't go passed bottom lip also but no thorough assessment completed"
"Not sure about this actually"
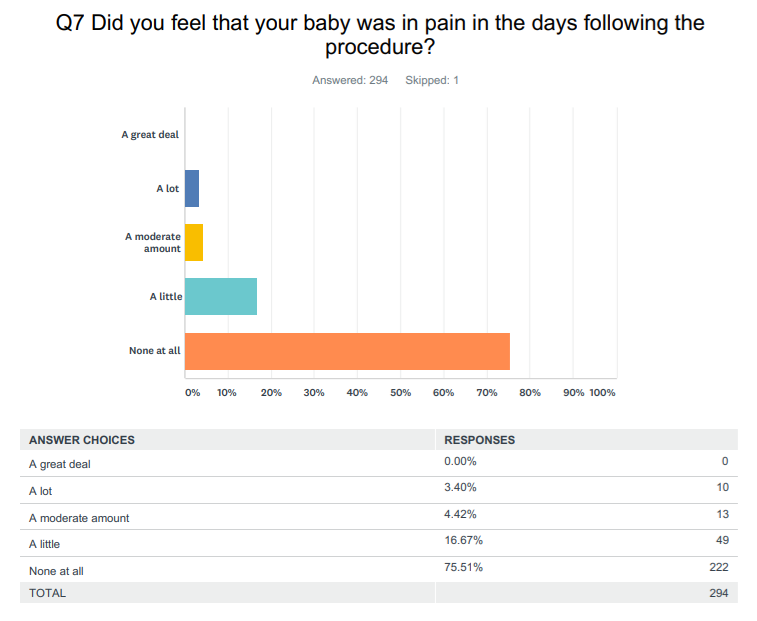
Q7- Did you feel your baby was in pain following the procedure? We're sometimes not very good at distinguishing when a baby is in pain. As late as the 1980s we actually conducted open heart surgery on infants without anaesthesia as it was believed that they didn't feel pain. It is just horrific to think of now. Some babies sleep through scissor tongue tie release so it may be reasonable to assume that those babies don't feel any significant pain during the procedure. Others are clearly very distressed at the procedure and continue to be so afterwards. A 2004 study found that 85% cried for approximately 20 seconds and that 0.5% seemed to be in pain for 24 hrs (Griffiths 2004). My survey found that 75% felt their baby was not in pain afterwards, 17% felt there was a little pain, and around 7% felt their baby was in moderate pain or a lot of pain.
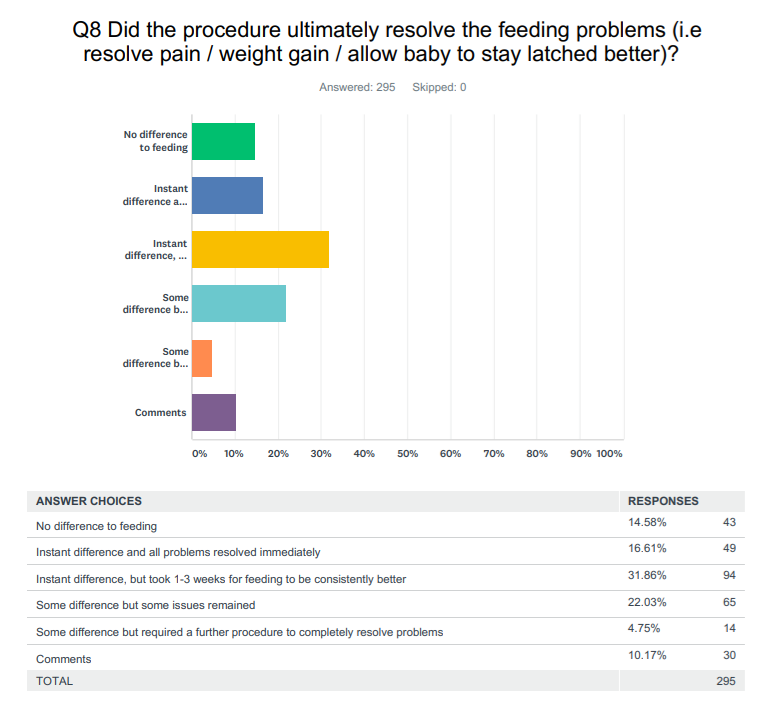
Q8 - Did the procedure resolve the feeding difficulties that it was designed to resolve? The survey found a very mixed bag here. Almost 15% felt that the procedure made no difference whatsoever. This is a very high number and the possibilities here are that: 1) the issue wasn't caused by a tie and the frenulum was misdiagnosed; 2) the tie wasn't adequately released. With the 2nd option here you normally see some kind of a change in feeding however. Re-attachment also would typically cause an initial improvement, but these families saw no difference. Almost 50% found that all the problems resolved in the weeks following the procedure. Nearly 5% had some improvement but required a second procedure which resolved the problems. This may have been due to incomplete release. 22% had some improvement. There is no way to tell from the survey if these babies were reassessed in order to see if the tie had been completely released, or whether they had a good surgical outcome and the remaining problems were unrelated to the tie.
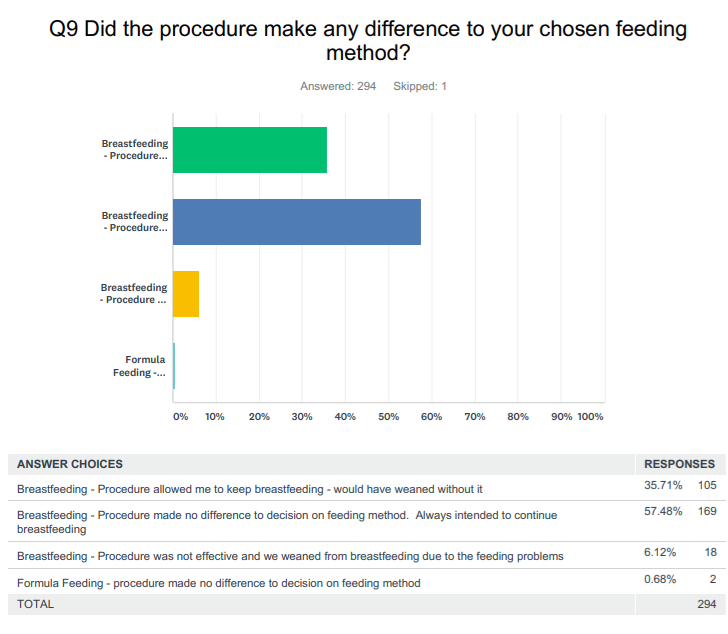
Q9 - Did the procedure make any difference to the decision to breastfeed or bottle feed? 36% of people felt that the procedure was vital to allowing them to continue breastfeeding and they would have weaned without the procedure. 6% felt that the procedure was not effective and therefore they weaned
to formula due to the feeding problems.
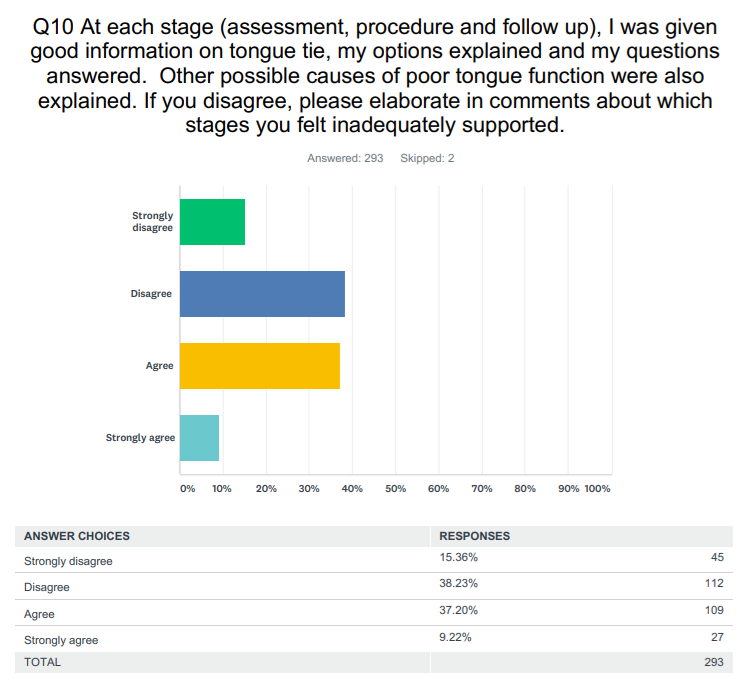
Q10 - In this question I asked if the families felt informed and supported throughout the entire process of assessment, the procedure and afterwards. The survey showed a very mixed experience here again. Only 46% felt that they were given adequate information and support throughout with 54% feeling they
were not. The comments expanded on this, e.g.
Best Practice
Overall I think what has come through in the survey consolidates what I am seeing in practice with clients, and clearly shows there is a lot of improvement that is needed in order to provide babies and their families with the care that they deserve. Best practice tells us that where there are breastfeeding difficulties which are not resolving through basic breastfeeding support, that mother and baby should be seen by a breastfeeding specialist (IBCLC, breastfeeding coordinator etc). If support is given by them and a tongue tie is suspected, the tongue should then be assessed on both function and appearance. In this way there should be a good identification of the tongue being restricted in some way. Referral can then take place. The clinic ideally will work with an IBCLC and will provide follow up support afterwards.
To look at how this affects the results I then filtered the survey to look at only the following cases:
Baby was seen by an IBCLC/breastfeeding coordinator (Q2 answered Yes)
Baby was referred by an IBCLC/breastfeeding coordinator (Q3 answered Yes)
Tongue was assessed by both function and appearance (Q7 answered Yes)
This gave a sample of 36 babies. In this sample 75% received follow up after the procedure (as opposed to less than 45% in the whole survey. 86% felt that they were given information about what to expect after the procedure (as opposed to 54%). Only 6% felt that the procedure made no difference (as opposed to 15%). I think this is a very stark difference - 2.5 times of a difference, and again consolidates the research that being seen by a specialist and assessing by function and appearance will better identify whether there is a tongue restriction and whether surgery is likely to make a difference. 42% said that it allowed them to keep breastfeeding and they would have weaned without the procedure (as opposed to 36%). This may reaffirm that IBCLCs/breastfeeding specialists are seeing more complex issues. Only 3% weaned to formula as the problems weren't resolved as opposed to 6% of the entire sample. Again this is very dramatic that following best practice meant that half as many people stopped breastfeeding. 70% of the sample felt that they were given adequate information and felt supported throughout (as opposed to 46%). To my mind, 70% is still very low, but it's still a big improvement.
I wanted to publish this survey in order to give some feedback to those who had participated. I have tried to keep my analysis as objective as possible. No comments have been included that personally identify any clinics, or healthcare staff. Overall however the survey does reaffirm my concerns that we are not adequately supporting breastfeeding families around tongue tie, either through providing access to specialised support, or through assessment and treatment of tongue tie.
The stats are better if you push for best practice however. So ask for it. If you are having problems that are not resolving through midwife/HV support it is advisable to see a specialist. Voluntary breastfeeding groups such as La Leche League have highly trained counsellors. They will not be able to assess a tongue tie but can provide high quality breastfeeding support and will tell you if you need further assessment or support. Within the NHS you can see the community lactation consultant if there is one in your area, or the hospital breastfeeding coordinator. The gold standard is to see an IBCLC who can provide the highest quality care, and they are available both in the NHS and in private practice.
Through this blog I have also linked my previous blogs on tongue tie assessment, other causes of tongue dysfunction and what to expect following release. These contain some of the information that I provide to my clients around tongue tie. As a region, we need to do a better job at supporting families around tongue tie so that only babies who need the procedure get it, those who get it get good information and that everyone gets the best breastfeeding support possible
If you have any questions about a consultation or would like to arrange to meet, please get in touch.
Important Information
All material on this website is provided for educational purposes only. Online information cannot replace an in-person consultation with a qualified, independent International Board Certified Lactation Consultant (IBCLC) or your health care provider. If you are concerned about your health, or that of your child, consult with your health care provider regarding the advisability of any opinions or recommendations with respect to your individual situation.
