I am an IBCLC (International Board Certified Lactation Consultant) in private practice in Northern Ireland and a La Leche League Leader with La Leche League of Ireland
A Tongue Restriction Isn't Always a Tongue Tie
A few weeks ago I wrote a blog about the differences between a tongue frenulum and a tongue tie. This is a follow on from that blog so If you haven't read it already I encourage you to read it first. The previous blog discussed what a tongue restriction is, and how it affects tongue function.
This blog will look at the role of bodywork and explain why a tongue restriction isn't always down to a tight frenulum. Other factors can be involved and many IBCLCs (International Board Certified Lactation Consultants) are now starting to question whether too many babies are having surgery, and if this is the correct intervention.
Whereas an anterior frenulum is normally quite visible and frenotomy (the procedure to divide the frenulum) has been done for a very long time, the concept of the posterior tie is more recent. Commonly posterior ties are diagnosed by pushing back on the floor of the mouth on the underside of the tongue.
Alison Hazelbaker IBCLC recently weighed in on the discussion on her blog. If you aren't aware of who Hazelbaker is, she is a important name in the world of tongue restrictions. She is the creator of the ATLFF tool which is used to functionally assess a baby's tongue and is the author of probably the most complete book on tongue-tie ("Tongue-Tie Morphogenesis, Impact, Assessment and Treatment"). As well as being a lactation consultant, Hazelbaker is a craniosacral therapist, so she understands both the tongue movement needed for breastfeeding and the effect of bodywork. In her blog, she said,
To my knowledge, no research has ever been done to verify that a restriction at the tongue-base that presents as a thick, shiny string under the mucosa is an actual tongue-tie. My experience as a structural therapist, and in the experience of many a bodyworker throughout the world, has shown that this type of tongue and/or mouth floor restriction resolves with simple bodywork; that the actual cause of this type of restriction is an acquired soft tissue strain pattern due to intrauterine or birth events.
http://www.alisonhazelbaker.com/blog/2015/9/1/modern-myths-about-tongue-tie-the-unnecessary-controversy-continues
Hazelbaker clearly states that in her belief tongue restriction can be caused by damage or strain to soft tissue (tendons, ligaments, muscles, nerves etc) either in the uterus or during birth, and can be resolved through bodywork - not surgery. This is what I wanted to explore a little in this blog, because it is something I don't see discussed regularly on local forums.
Soft Tissue Tongue Restriction
So what is Hazelbaker talking about when she mentions soft tissue strain, and how could it affect a baby's tongue? This is where we need to dip into a bit of anatomy, which I will try to keep as brief as possible to prevent this blog becoming 30 pages long! Stick with me - it will become clear.
A baby's complex suck-swallow-breathe sequence requires the function of 6 cranial nerves, 6 cervical nerves and a few thoracic nerves coordinating 31 muscles in the lips, cheeks, tongue, jaw, chin, soft palate etc. That's a lot of soft tissue!
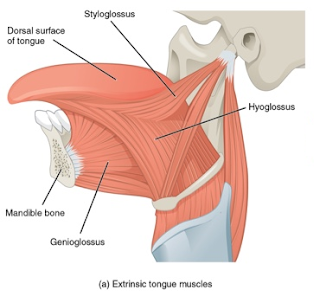
This image shows some of the muscles of the tongue. Muscles are usually labelled based on where they attach. Glossus refers to the tongue, so tongue muscles will have glossus in their name. Look at where some of the tongue muscles attach. The muscle labelled Styloglossus attaches high up on the jaw bone close to the ear. The large muscle below that labelled Hyoglossus attaches the tongue down to a thin bone in the neck called the Hyoid. The genioglossus attaches the tongue to the chin. Note how far forward the Hyoglossus and genioglossus muscles attach to the underside of the tongue.
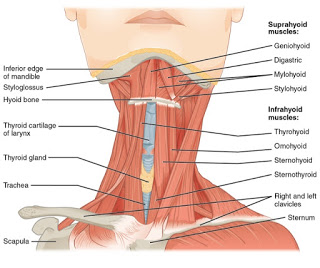
The Hyoid is more clear in this image of the neck. You can see how multiple muscles from the head and face attach to it above and then if you look at the underside of the bone you can see muscles attaching to the shoulder and the sternum.
The CNX.org anatomy pages (where these images are from) describes the hyoid bone as:
a horseshoe-shaped bone that functions as a solid foundation on which the tongue can move
The hyoid is a little unusual in that it doesn't attach to any other bones, but instead floats, held in position by the muscles above and below. So, we have a bone which is the foundation of the tongue which is held in position by muscles above and muscles below.
Are you starting to see how a strain on a muscle attached to the hyoid could affect the tongue?
The uterus is a pretty tight place at the end of a pregnancy and a baby who remains in one position for some time can be "moulded" into specific positions. That might cause something like a baby's feet to be turned inwards or it could be that the baby's head is leaning to the side a little for example. A baby who spends their final few weeks with their head tilted can have a slight tightness and shortening of muscles on one side of the neck compared to the other. That makes sense doesn't it? If we sleep at a funny angle for only a few hours we can feel the muscle tension when we wake. So look at the neck image again and apply it to a baby who has their head tilted slightly to the side at birth. Think of how that might affect the hyoid and the tongue. Perhaps grab yourself a glass of water and drink with your head straight and then drink with your head tilted, to get an idea of how it affects the ability to "latch" to your cup and to drink. If I tilt and drink I feel a lot of tension in my upper lip. I have to tighten my lips around the cup rim in order to manage the flow of liquid. Mmm... tightening and using lips to maintain latch - isnt that what a tongue restricted baby often does? That tightening and using lips to grasp the breast causes pain and friction for mum and baby (nipple trauma and sucking blisters for baby) and often poor milk transfer. When we pour from a glass we manage the flow of liquid by the tilt of the glass. I imagine if the water started gushing (like during a letdown) I would struggle to manage it. All typical behaviours with tongue tied babies.
A 2008 study (Rubie, Griffet, Caci, Bérard, El Hayek, Boutté) of 1001 babies found that 10.7% of babies that they studied had Moulded Baby Syndrome. Moulded Baby Syndrome was classified as any of the following:
- plagiocephaly (where the skull may be flattened in one area or asymmetrical )
- torticollis, (head tilted to the side and baby often looking in the other direction)
- congenital scoliosis (a curving of the spine - this can be mild and not very noticeable)
- pelvic obliquity (misalignment of pelvis)
- adduction contracture of a hip (misalignment of hips)
- malpositions of the knees or feet
An assymetrical skull can change the tension of one side of the tongue compared to the other by having assymetrical attachment points for the muscles. A slight curving of the cervical spine could have an effect much like tilting your head to the side, where the muscle tension on the hyoid is assymetrical. Assymetry of the pelvis and hips results in assymetrical tension on the spine, shoulders, neck and head. All of which can affect the latch.
The study found that moulding was 6 times more likely after an instrumental birth, 2.7 times more likely if baby was a breech presentation, 10 times more likely if there was low amniotic fluid, 1.98 times more likely in boys and 1.65 times more likely in a preterm birth. The instrumental birth figure jumps straight out. 6 times more likely! Think of the process of what happens during an instrumental birth compared to a normal birth. A baby is designed to be pushed through the birth canal. The bones of the head should mould to allow delivery and then over a short period after birth, they readjust position. Vaccum, forceps and often also ceseareans pull a baby out by the head. Is it surprising that the head and neck might feel strain? Think of how those tongue muscles attach high on the jaw where forceps may press, or how the abnormal moulding caused by the suction of a vacuum may change the position of skull bones. A cesarean where a baby is lifted out by the head creates pressure to the base of the skull and the neck which can also compress nerves and muscles in the neck, including those associated with the hyoid.
So, how much of an issue could that be here in Northern Ireland? Well, the birth statistics for Northern Ireland in 2014 show that 12.9% of deliveries were assisted by instruments and 29.1% were cesarean deliveries. Moulding isn't just an issue with assisted deliveries. Even very fast or very slow unassisted vaginal births can cause abnormal moulding and the other figure to consider is the induction rate. The induction rate was 33.4%. Induced contractions are not the same as natural contractions. They do not build in the same way and do not have the same pattern. What effect do inductions have on normal/abnormal moulding during birth? Perhaps it isn't surprising that the study found so many babies with Moulded Baby Syndrome. Perhaps it also isnt surprising that there is a debate over how many babies are tongue tied, and whether the rate is rising. We don't have figures for Northern Ireland, but the instrumental delivery rate in England in 1953 was 3.7%, and in 2013 it was 12.7% so the instrumental birth rate is certainly rising.
Clearly tongue ties due to a tight frenulum (an anatomical tongue tie) exist, and I discussed them more fully in the previous blog. The gene associated with tongue-tie has been identified and for these babies, a frenotomy (the surgery to divide the frenulum) can save a breastfeeding relationship as well as have lifelong impacts on the oral and facial development of the child. Locally I think there is plenty of awareness on forums about the option of frenotomy. Not all tongue restrictions are due to anatomical reasons however. Some tongue restrictions can be due to other structural tensions and can be resolved by releasing those tensions. A baby may have a normal stretchy mucosal frenulum, but also have structural muscle tension making the frenulum seem more restrictive than it is. A baby who is having breastfeeding difficulties may have the anterior frenulum blamed, only to later find that a frenotomy of that frenulum makes little difference.
In most cases abnormal moulding or slight torticollis resolves itself over time, and so for most dyads, breastfeeding difficulties caused by this also resolve with good support. The study discussed above found that 77% of plagiocephaly and torticollis were resolved within 8 weeks with parental interventions like careful positioning of babies. Tummy Time, for example can be a very helpful breastfeeding intervention as it mobilises the throat and tongue and it's interesting that laid back breastfeeding (which many people find is a very easy position with a newborn) is a tummy time position. Perhaps this natural resolution of tensions is where the idea of a tongue tie stretching over time came from - from babies whose tongues had structural restrictions (rather than anatomical) which naturally resolved.
For some babies however, tensions are more persistent, as the remaining 23% in the study show. Even with those that will resolve in the first 2 months, there is a breastfeeding mother and a baby who may struggle with painful feeding, mastitis and poor weight gain during that time. For some dyads, waiting for these structural issues to resolve is not a option and they need help quickly. For those babies, bodywork can be helpful. By the term bodywork, I mean gentle manual therapies which release soft tissue restrictions, such as cranial osteopathy, craniosacral therapy or paediatric chiropractic. Many IBCLCs who work extensively with tongue-tie recommend bodywork for babies with a tongue restriction and then later reassessment of tongue function before referring for a frenotomy, as the bodywork may resolve the restriction. Even if it doesn't fully resolve the restriction some practitioners feel it makes visualisation of the frenulum easier if a frenotomy is needed.
Tongue tie care in Northern Ireland is very inconsistent and perhaps some of this blog and the previous tongue tie blog explains why locally mothers and babies have such different results from having a frenulum divided. Some mothers talk about how a "quick snip" resolved all their problems, others found that it didn't help, or maybe made things worse. Some dyads are referred for surgery (and frenotomy is a surgical intervention) without a proper breastfeeding assessment and with limited, if any follow up afterwards. Most babies do not have a functional tongue assessment. Some mothers are given information around bodywork whereas others don't get any information about this. Some are given limited information about the surgery and others have a full care package where a lactation consultant works with a surgeon, consulting together, with risks and possible outcomes fully discussed. Some families travel a considerable distance for this kind of care while others don't know it exists. In each situation is a mother and a baby who are having some kind of feeding problems and usually a mother who is scared and worried about the thought of someone putting scissors in their tiny baby's mouth.
If you are having breastfeeding problems and are concerned about whether a tongue restrictions part of the issue, contact a lactation consultant (IBCLC) or accredited breastfeeding counsellor who can help you research all the options. The first stage in any breastfeeding support should be looking at ways to optimise latch and milk transfer, but it should also involve a thorough history of factors in pregnancy and the birth. It's important to remember that it's the minority of babies who have tongue restrictions and the vast majority of breastfeeding issues are related to other factors like latch / flow / positioning / frequency of feeds etc. If a suck issue is suspected however, a functional tongue assessment should be done. At present this needs to be done by an IBCLC (International Board Certified Lactation Consultant) or an appropriately trained HCP (healthcare professional). If the tongue is restricted the family should be provided with all the options that can help. Any subtle structural assymmetries of the head and body should be considered and the options provided to the family, including bodywork. If the parents decide to have a frenotomy, risks and benefits and follow up care should be discussed. Tongue tie division (frenotomy) is a surgical procedure. It may be low risk but a baby experiences much of the world through their mouth and we should be cautious about interventions if they are not needed, and we should take as much care as possible and provide relevant information if they are needed.
Look for a breastfeeding professional who will look at the whole picture of you and your baby. A quick snip isnt always the answer to a tongue restriction.
If you have any questions about a consultation or would like to arrange to meet, please get in touch.
Further Reading
Tongue Tie
http://www.alisonhazelbaker.com/blog/2015/9/1/modern-myths-about-tongue-tie-the-unnecessary-controversy-continues
Alison Hazelbaker. 2010. Tongue-Tie Morphogenesis, Impact, Assessment and Treatment, Aidan and Eva Press
ABM (Academy of Breastfeeding Medicine) Protocol - http://www.bfmed.org/Media/Files/Protocols/ankyloglossia.pdf
ATLFF (Assessment Tool for Lingual Frenulum Function) - https://www.med.unc.edu/pediatrics/education/current-residents/rotation-information/newborn-nursery/hazelbaker_frenum.pdf
Video of Functional Assessment of the Tongue - http://m.youtube.com/watch?v=-4G-yV11iYA
Anatomy of the Tongue, Neck and Head
Images from blog: http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@6.27:76/Anatomy_&_Physiology
Video of Tongue Muscles & Hyoid Bone - http://youtu.be/NC3_RNRAvQc
Studies referenced above
http://www.researchgate.net/publication/23258426_The_moulded_baby_syndrome_Incidence_and_risk_factors_regarding_1001_neonates
http://www.orthopaedicsandtraumajournal.co.uk/article/S0268-0890(02)90232-X/abstract
BodyWork & Breastfeeding
http://kellymom.com/bf/concerns/child/cst/
http://www.lalecheleague.org/llleaderweb/lv/lvaugsep01p82.html
http://www.spz-frankfurt.de/fileadmin/user_upload/Website/Fuer_Profis/Publikationen_Vortraege/Therapiestudie_Osteopathie.pdf
http://www.cranialosteopath.com/newborns.html
Birth Statistics
http://www.birthchoiceuk.com/Professionals/BirthChoiceUKFrame.htm
http://www.birthchoiceuk.com/Professionals/InstrumentalHistory.htm
Important Information
All material on this website is provided for educational purposes only. Online information cannot replace an in-person consultation with a qualified, independent International Board Certified Lactation Consultant (IBCLC) or your health care provider. If you are concerned about your health, or that of your child, consult with your health care provider regarding the advisability of any opinions or recommendations with respect to your individual situation.
