I am an IBCLC (International Board Certified Lactation Consultant) in private practice in Northern Ireland and a La Leche League Leader with La Leche League of Ireland
"Everyone tells me something different" - Feedback from Parents
Earlier this month I was at Breastival Belfast - a celebration of all things breastfeeding held in the Ulster Museum, Belfast during World Breastfeeding Week. It was a great event with lots of speakers, stands, workshops, panels and general info about breastfeeding. I did a presentation on the 4th Trimester and I also had an exhibition stand on the day. The theme of WBW 2019 was Empower Parents Enable Breastfeeding and as part of the stand I asked people to participate in a word cloud giving their thoughts on what was needed locally to Empower Parents and Enable Breastfeeding. This is the wordcloud from the day.
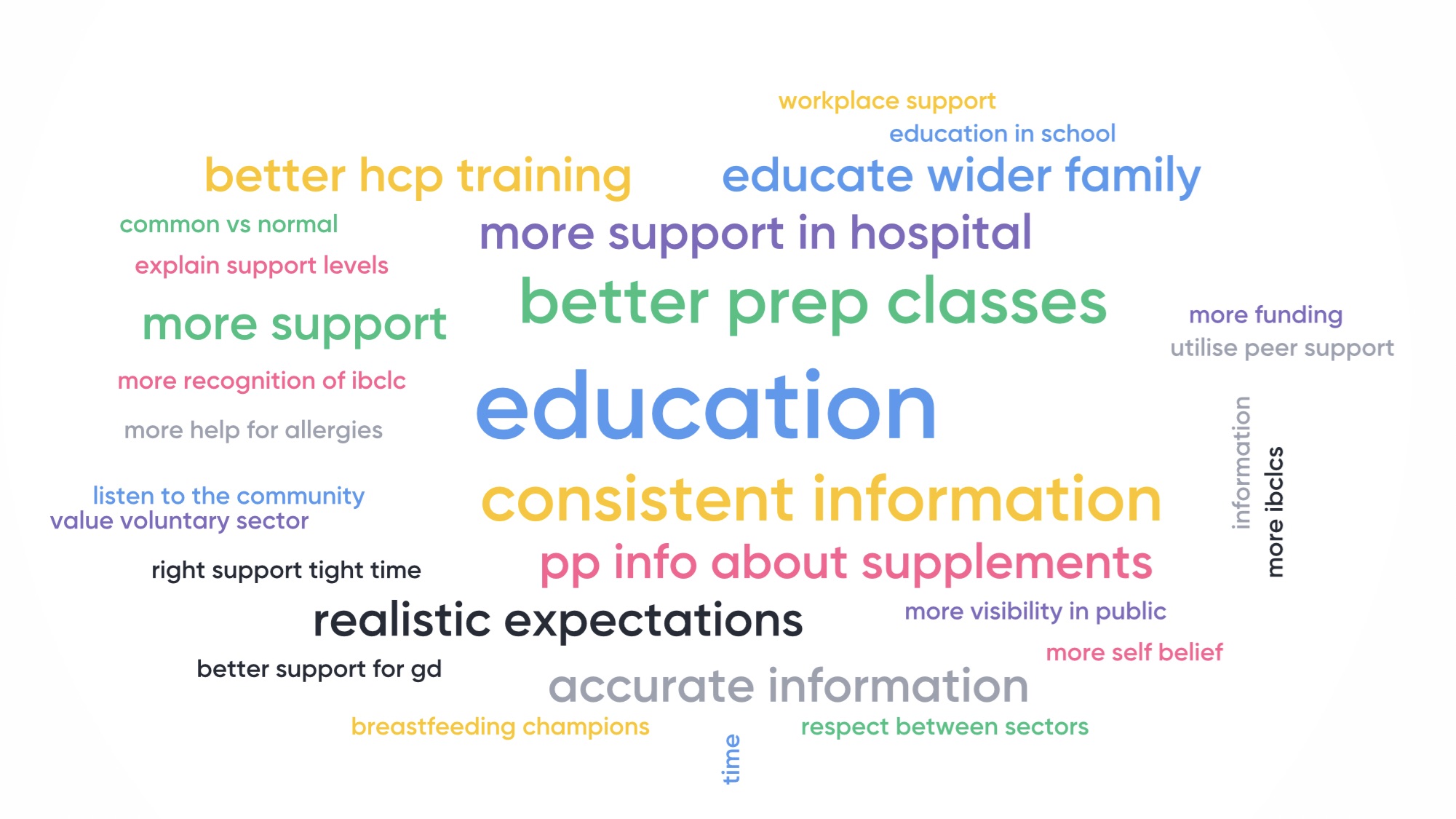
It's very clear what parents are asking for here - at least to me. They are asking for better informed professionals offering better information to the family and to the public. Education is clearly the most common word, but many of the other words/phrases also link into education. I see linkages looking like this:
1. Education for HCPs. This may be about technical information on breastfeeding (the biomechanics), but it may also be better training for how to deliver support or education classes.
This is indicated by the following phrases:
- Better HCP training
- More Help for Breastfeeding a Baby with Allergies - Many parents had been told that dairy proteins do not pass in breastmilk - which is patently false and demonstrated in research.
- Better support for women with Gestational Diabetes who want to breastfeed - one mum told me about vague answers to questions when she queried about need for supplements after birth
- Better preparation classes - This is also picked up in the Education for Parents. Parents did not feel that the antenatal breastfeeding classes give them the information they needed. It focused on the value of breastfeeding but not the how to's.
- Information about Supplements - Many parents needed to use some supplementation in the early days and felt there was very poor support around this. They were told to give supplements but not given any plan to wean off, not told that it could be a temporary measure. Some were not told to express in order to allow them to wean off the supplements again. Many received no information about paced feeding or guidance about how to maximise breastmilk and minimise the supplementation.
- Consistent Information - Parents told me that they heard different advice from each midwife they saw
- Accurate Information - As above parents got inconsistent advice, some of which was accurate and some was very outdated.
2. Education for Parents
- Common vs Normal - This comment was in relation to NI being a formula feeding culture and parents needing to know that what is common (feeding 3-4 hourly for example) isn't necessarily normal
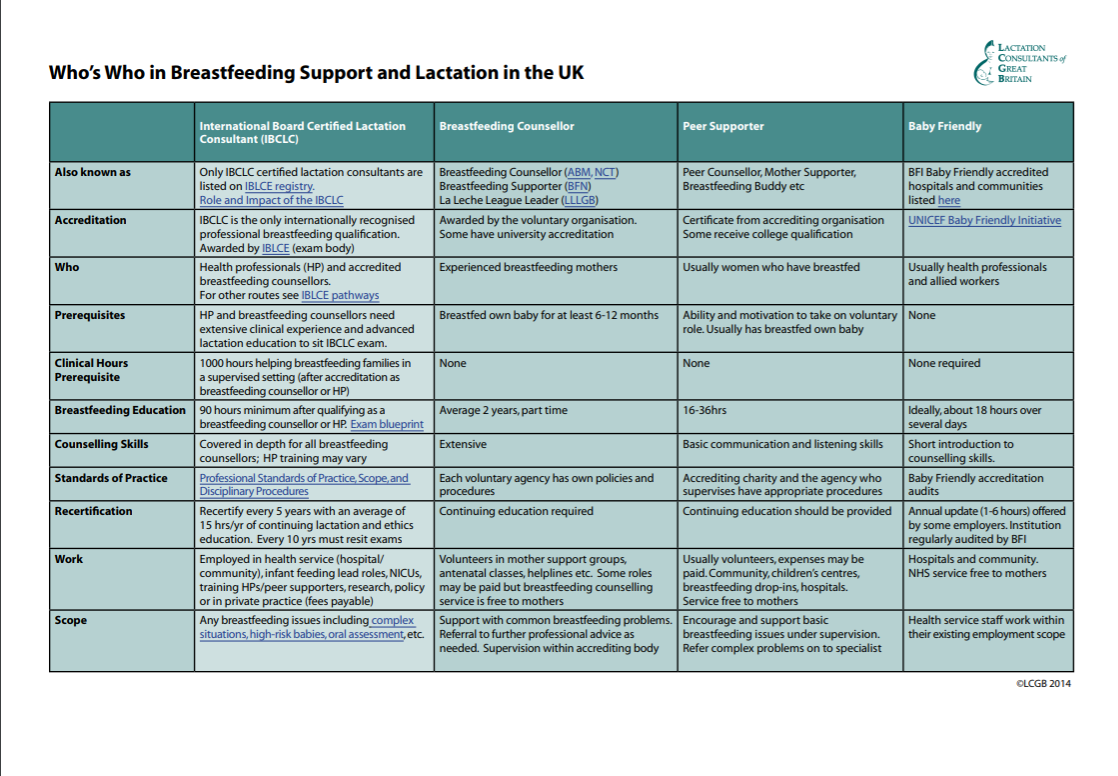
- Explain Support Levels - Parents want to know more about who is supporting them and how well trained they are
- Realistic Expectations - Parents did not feel that the antenatal breastfeeding classes give them the information they needed. It focused on the value of breastfeeding but not the how to's.
Who educates the parents? Partly this should come through public health messaging on billboards, media campaigns etc, but on the whole this kind of information comes through our HCPs, our family support workers etc - and that takes us full circle back to the question of why we are getting inconsistent information from HCPs.
Before we get into that specifically I can do something to explain the support levels. The chart below has been put together by LCGB (Lactation Consultants of Great Britain) to show the training and support offered by HCPs (Baby Friendly training), peer supporters, breastfeeding counsellors, IBCLCs. The original pdf is available on the LCGB website here.

Why are families getting inconsistent or inaccurate advice?
I would say that without a doubt the one phrase I hear more often than any other in consults where the baby is under 2 weeks old is, "every midwife or Dr tells me something different". I'll give you a few examples of things I hear regularly.
One baby I met recently was very sleepy in the 24 hours following birth. The mum was concerned that he wasn't waking to feed. She commented to midwives several times over the first 12 hours that her baby wasn't waking to feed. She was told "Don't worry. Your baby was born with his own lunchbox". This then led to her being pressured to give supplements a few hours later when a different midwife told her that her baby had to feed immediately.
A mum who in extreme pain throughout each feed in the first few days was told this kind of pain was normal by her midwife and that her own experience was that she had to bite down on a facecloth and cry through feeds for the first 2 weeks. Is this support? Others correctly say this is not normal.
Some mums have been told that newborns never feed for comfort and only feed because they need milk. This, of course, is nonsense. Babies feed for multiple reasons and much of it is not about nutrition. I have actually had a client who was told that babies only comfort feed after 8 weeks. I can only assume that this was a bumbled way of telling the mum that feeding is important for building milk supply in the first 6 weeks, and the message was confused either due to poor communication or lack of real understanding of breastfeeding. In contrast other midwives are telling mums that their baby is just using them "as a dummy" - a phrase that is frequently repeated back to me at consults.
Women are still told frequently to feed for 20 mins on one breast because of hind milk. See my series of blogs here on why this is outdated. The next midwife that person sees might tell her to swap sides and topup.
I have heard women told that their milk mustn't be of good enough quality due to low weight gain - with no good advice on increasing milk intake (see blogs here on weight gain concerns).
Just today I was told my a mum that her midwife told her that some babies just don't want to breastfeed - they just aren't interested in breastfeeding. Where this idea came from is bewildering and clearly is simply a justification for behaviour that the HCP just can't understand. Babies are hard wired to breastfeed. They have reflexes which cause them to gape and latch involuntarily when placed at the breast. They instinctively crawl to the breast to latch on if laid on their tummies. If they are unable to latch it is because something is interfering with their ability to follow through with these instinctive behaviours.
I have repeatedly heard information on allergies which is not backed up by research, and over and over again women tell me that the breastfeeding classes did not give them the preparation and expectations that they needed. I agree that it doesn't - which is why I created an online preparation program which I designed to meet that gap and to really give the How To's, the Realistic Expectations and Trouble Shooting info that parents need. Please do share this program with friends that you have if you have found my blogs helpful. I have tried to keep it low cost but providing really comprehensive preparation with over 3 hours of information and videos.
So Why is This Happening? Do our HCPs have the right information and training?
In 2016 the WBTi (World Breastfeeding Trends Initiative) UK report was published. This is their chart on training for HCPs.
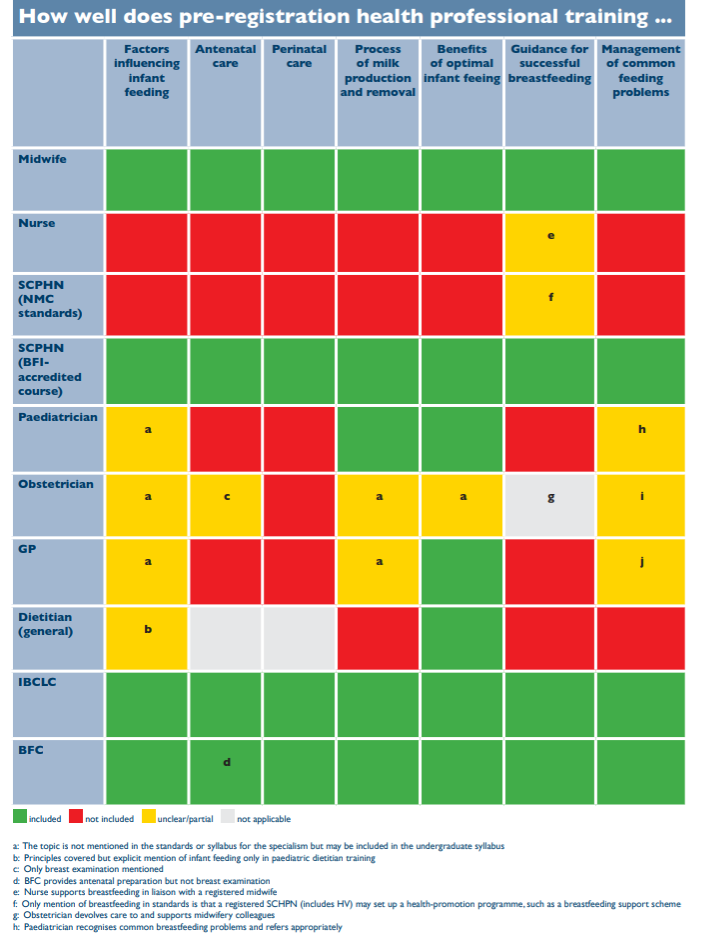
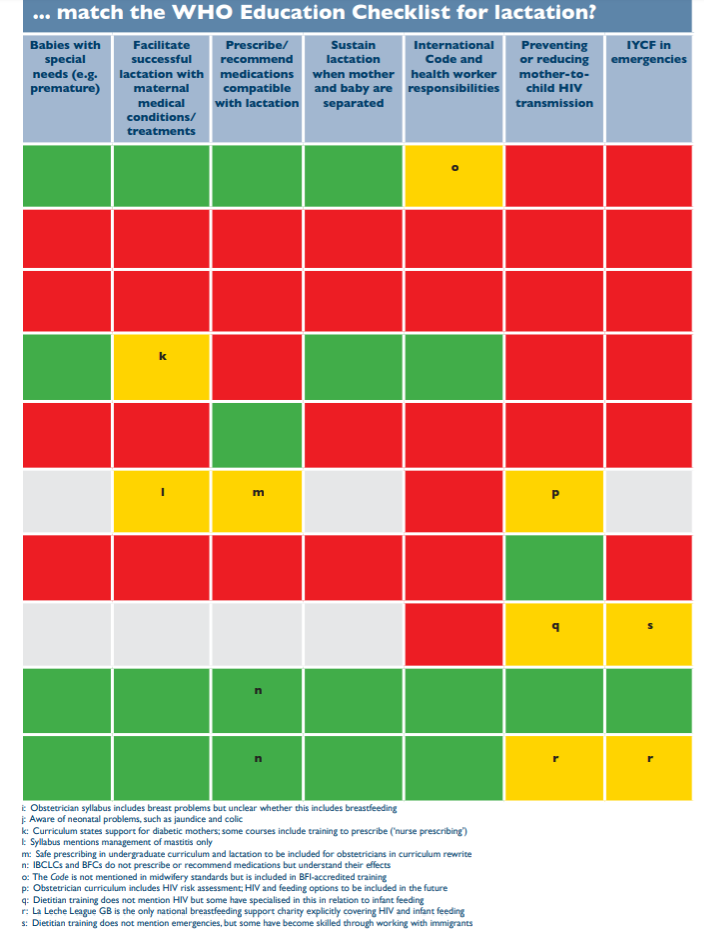
The original report can be found here and the chart is in Indicator 5 (Pages 30-31). The SCPHN row refers to Health Visitors. As of now (August 2019) we in NI do not have any BFI accredited HV training courses. Looking at the chart midwives look to be very well trained in breastfeeding support - so why is it that around 60% of women begin breastfeeding in NI but by discharge the number has dropped to approx 45%? That's almost 20% drop in anything between 6hrs and a couple of days when women are in the hospital system with easy access to midwives. Why is this happening if midwives are well trained in "Guidance for successful breastfeeding" and "Management of common feeding problems"?
Why have the rates fallen to 35% within the first 10-14 days when women are having midwives visit every couple of days during those times? Few other countries can boast that 100% of their hospitals are BFI accredited and they have frequent home visits from birth - 2 weeks, yet most other countries have much higher breastfeeding rates than we do. What is happening with our training and support?
On training, the WBTi report states,
the breastfeeding knowledge included tends to be theoretical rather than the practical aspects of enabling mothers to initiate and continue breastfeeding.
I think every mother who has ever breastfed will tell you there is a difference between theoretical knowledge and practical experience. Most of us who read and researched about breastfeeding in order to get ourselves and our babies "off to the best start" will happily state that we learned much more by actually breastfeeding than we learned from reading about breastfeeding. Breastfeeding is a right brained, hormonal, experiential learning experience. I've worked with many HCP mums who realised this as well when they had their own babies.
Theoretical knowledge only goes so far, and it doesn't cover all circumstances.
This feedback that information given around infant feeding is inconsistent isn't new. The NICE Guidane on Maternal & Child Nutrition (PH11) noted:
that some dietary advice given by those responsible for the care of mothers and pre‑school children is not evidence‑based and that information provided by health professionals is not always consistent.
It recommended further training.
Crucially though something which I think isn't well addressed in training is the personal experience of the HCPs themselves. Our society has 35% breastfeeding rates at 10-14 days. Our HCPs are part of our society and it's reasonable to assume that 65% of those midwives and HVs who have given birth have not breastfed past 14 days. It's reasonable to assume that 40% of them have never breastfed at all. It's reasonable to assume that many of them had difficulties and were not well supported to continue. We also know that shift working patterns actually increase the risk of pre-term birth so HCPs who are regularly working shifts may actually have a higher percentage of preterm births and subsequent feeding difficulties. What do we know about how this affects women and their attitudes to breastfeeding?
We know from the last UK Infant Feeding Survey (2010) that almost 90% of women who give up in the first 2 weeks didn't want to. We know that women who wanted to breastfeed and were unable to feed for as long as they wanted are 2x more likely to suffer from post natal depression. A 2000 study (Mozingo et al) found that stopping breastfeeding before they wanted left women with a,
sense of failure, guilt, or shame and [they] had lingering self-doubts about not continuing with breastfeeding
We all deal with failure, guilt, self-doubt in our own way, but there is no doubt that if we don't process those feelings and our experience fully then we are often unaware that how we discuss or refer to it can really affect the person we are talking to. Breastfeeding support is primarily counselling. It's not about fitting a mouth and a breast together according to what a textbook says. It's working with a mum recovering from birth, perhaps in pain, who may have stitches, bruising, bleeding, feels vulnerable and tired. It's about working with a baby who may have had a difficult birth and be equally bruised or tired, has had drugs interfere with the normal process of birth, has had some separation from mum and who's head is sore. It's about helping the family deal with the fact that their expectations of breastfeeding may not match up to reality. Their expectations of sleep and baby behaviour may not match up to reality. They may be confused, anxious and they all just want to do the best for their baby. This is about counselling. Meier & Davis (1997) says that
in no other profession does the personality and behavior of the professional make such difference as it does in counseling.
Self awareness is key. Are HCPs who have had a difficult breastfeeding experience aware of their own biases around that? Do they want to "save" other mums from what they experienced? Do they still value breastfeeding? Do they want to support and help other women to breastfeed or does that tap into their own feeling of failure and guilt? When they talk about their own experience, are they doing it for the benefit of the person they are counselling - or for themselves? Was it helpful to the mum asking if her pain was normal to hear that her midwife had bitten on a flannel for 2 weeks? Was it helpful for another mum who had got a blocked duct to be told by her Health Visitor that she had experienced rigours when she had mastitis? Is it helpful to the mum who is struggling to hear, "Some people just can't breastfeed. I couldn' t do it"? Is that about the mum or the HCP? Is it what the mum who was asking for help needed?
A basic rule of counselling is that we don't give our own experiences. In order to be able to listen actively and concentrate on the person rather than the thoughts the situation is bringing up internally (I remember that happening to me) we need to have processed our own experience. Many voluntary organisations who train breastfeeding counsellors (e.g. La Leche League, NCT) have reflective sessions and debriefing within their training so that counsellors don't carry their own biases into a support environment. This is not in place for HCPs.
So where parents overwhelming brought up the topic of education at Breastival this year, I wonder if it's time for the NHS to also treat their HCPs breastfeeding experiences with concern in regard to their role as counsellors. Yes the WBTi report is very clear that there are significant gaps in education, but even where education is most comprehensive we are having support issues. So perhaps it is about more than breastfeeding education. Maybe part of the solution is that training courses need to be expanded to Support the Supporters. Counselling starts with reflection. Where is the debriefing time when a midwife or HV returns to work after having her own baby? What about asking her how she feels about supporting other women to breastfeed? Does she want to?
No doubt there is no money to help HCPs in this way. But I wonder how it could help with breastfeeding support if there was...
Just a thought.
If you have any questions about a consultation or would like to arrange to meet, please get in touch.
Further Reading
1. LCGB Who's Who Chart - https://lcgb.org/wp-content/uploads/2015/01/Whos-Who-in-Breastfeeding-in-the-UK-2014.pdf
2. WBTi UK Report 2016 - https://ukbreastfeedingtrends.files.wordpress.com/2017/03/wbti-uk-report-2016-part-1-14-2-17.pdf
3. NICE Guidance on Maternal & Child Nutrition - https://www.nice.org.uk/guidance/ph11
4. Infant Feeding Survey 2010 - https://sp.ukdataservice.ac.uk/doc/7281/mrdoc/pdf/7281_ifs-uk-2010_report.pdf
5. Mozingo, Johnie N. PhD, RN; Davis, Mitzi W. PhD, RN; Droppleman, Patricia G. PhD, RN; Merideth, Amy MSN, (2000). "It wasn't Working": Women's Experiences with Short Term Breastfeeding. The American Journal of Maternal/Child Nursing: May-June 2000 - Volume 25 - Issue 3 - p 120-126
Important Information
All material on this website is provided for educational purposes only. Online information cannot replace an in-person consultation with a qualified, independent International Board Certified Lactation Consultant (IBCLC) or your health care provider. If you are concerned about your health, or that of your child, consult with your health care provider regarding the advisability of any opinions or recommendations with respect to your individual situation.
