I am an IBCLC (International Board Certified Lactation Consultant) in private practice in Northern Ireland and a La Leche League Leader with La Leche League of Ireland
Breastfeeding, Food Intolerance & Allergy
Suspicions, investigations and diagnoses of allergies is pretty high in our babies these days. The NICE guidance on allergy states that cows milk protein allergy alone affects 7% of formula fed and combination fed infants. Given that we know from the infant feeding survey that only 13% of babies are exclusively breastfed at 6 weeks in Northern Ireland (23% across UK) , many breastfeeding mothers are also dealing with allergy. The 7% are diagnosed allergies. Many more babies and children suffer delayed food reactions of varying degrees (sometimes mild constipation or eczema which are not investigated) and when these are added in, it is estimated that 15-25% of infants and young children have some kind of food sensitivity /allergic reactions (Figure from "Baby Poop: What Your Paediatrician may not Tell you" -see further reading.) Given that is the case, it's understandable that many mums wonder about intolerances and allergies when their baby is fussy. Often when mums post on internet groups about their fussy baby they get many comments suggesting she remove dairy from her diet. Many mums have removed dairy without any real investigation into whether a breastfeeding problem is linked to the fussy behaviour, or whether it may be developmental. There seems to also be a lot of misunderstanding about what intolerance or allergy is, and also how it relates to breastfeeding so I thought that in this blog and the next, I'd try to cover about few basics about them.
Lactose Intolerance
Firstly lets start with the idea of lactose intolerance since there is a lot of population misunderstanding about dairy and lactose intolerance. Intolerance is not allergy. Intolerance means that the food cannot be metabolised / broken down and used by the body.
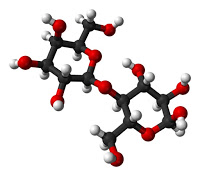
Lactose is a sugar. Lact-ose - literally means milk sugar. It is a made up of 2 other simple sugars (galactose and glucose), is contained in all mammal milks and is a very rich source of energy for infant mammals. It makes up approximately 7% of Breastmilk by volume and provides about 60% of the energy in Breastmilk. Since it is the main source of energy it is vital that a baby can digest lactose and it is designed to rapidly grow the human brain.
So we have a normal milk sugar called lactose in milk (both human milk and other mammal milk, including cows) which enters the baby's gut when the milk is drunk. Babies (and all infant mammals) produce an enzyme in their gut called lactase. The job for lactase is to break the lactose down into those 2 components of galactose and glucose, which can then be easily used as energy by the body. Lactose intolerance is the inability to break down lactose. It happens when the body does not produce lactase to break down the lactose.
Most mammals infants produce lots of lactase as they obviously need to break down the lactose milk sugar which is their major energy source. As they get older they produce less and less lactase. This is by design and is a natural part of the weaning process. An animal moves to an adult diet, it no longer requires milk and therefore doesn't need the ability to digest milk. So they gradually produce less lactase, they drink less lactose and they naturally wean to an adult diet. This is also the case in most of the human world, BUT not in those of European descent. Dairying has been a big part of culture in this part of the world for thousands of years. We know that very large dairies were in place in Ireland 5000 yrs ago. Around the same time as the rise of dairies we developed a mutation in our genes which allowed us to continue to produce lactase and therefore digest milk, into adulthood. It was probably an important source of nutrition at that time if there was enough selective pressure to mutate the gene. So for several thousand years people from this part of the world have produced lactase both as infants and adults, and are able to digest lactose throughout their life.
It is extremely rare for a baby to be born with a lactose intolerance as it would leave that baby unable to digest any milk. That would be a biological disaster for a mammal, so if someone suggests to you that your baby may be lactose intolerant, it is extremely unlikely to be true.
It is possible in some circumstances for a baby's gut can to be be overwhelmed by lactose however and for symptoms of lactose intolerance to appear. There are 2 common conditions where this can happen:
- Baby or mum has had antibiotics or a stomach bug. Lactase is produced by the border cells of the small intestine. Both antibiotics or a GI infection can destroy the healthy gut bacteria lining the gut and in doing so the border cells can be damaged. Until the cells are repaired there may not be enough lactase created to digest all of the lactose that a baby drinks. It is known as temporary lactase deficiency and continues until the gut border is healed and the cells are creating lactase efficiently again. Breastmilk has components which help to heal the gut!
- If mum perhaps has a oversupply of milk (maybe due to expressing or tandem feeding or swapping sides more often than her particular baby needs), or is scheduling feedings and feeding from very full breasts each time, it can mean that a baby gets more lactose than needed and that can overwhelm the amount of lactase in the gut leading to colicky symptoms. Lactase is still produced, just not in the amount needed to deal with the overload of lactose. So lactase breaks down the lactose that it can, but lots of lactose molecules are left over and not digested This is common and easily resolved just by a little breastfeeding management around feeding frequency. See my previous blogs on Foremilk/Hindmilk, Oversupply and Fast Letdown.
Lactose attracts water so the result of lactose not getting broken down in the gut is comparable to eating a lot of dried fruit, prunes for example. It pulls water into the intestine to join the lactose. This creates a watery solution which passes through the gut very quickly. It also means there is a lot of sugar to be fermented by bacteria in the gut. The result is a baby who is colicky, gassy and has green slimy stools.
Occasional green stools are nothing to worry about. It is likely that all breastfeeding mothers have times where their baby slept unusually long at night and fed from a very full breast in the morning and resulted in a green stool.
If you are concerned that your baby is having frequent colicky, gassy, green stool symptoms, contact a breastfeeding counsellor or lactation consultant (IBCLC). If it is caused by an overload of lactose, altering your breastfeeding daily rhythm is usually all that is needed. This is not a true intolerance and you switching to lactose free dairy will not make any difference. Your milk will still contain lactose, because it is produced in your breasts and that is what your baby needs for his rapid brain growth.
Food Allergy
In contrast to intolerance, where there is an allergy the immune system is involved and reacts to exposure. Usually in dairy it is due to exposure to cows milk proteins, not lactose. Commonly allergies are categorised into IgE-mediated reactions and non-IgE-mediated reactions.
IgE stands for Immunoglobulin type E and is one of the 5 subtypes of antibodies which our bodies make (IgA, IgD, IgE, IgG, and IgM). IgE antibodies are mostly found in the lungs, skin and mucous membranes. IgE antibodies are implicated in dietary allergy and have a fairly immediate reaction - often within minutes of eating the allergen and can range from skin issues like hives to hayfever like symptoms of streaming eyes and nose, or respiratory symptoms like wheeze and cough to life threatening anaphylaxsis symptoms. Most people recognise this reaction as an "allergy"
Non IgE-mediated-reactions are delayed reactions which do not involve IgE antibodies. Non IgE reactions can appear from a couple of hours to 2-3 days after foods, which makes identification and diagnosis much more tricky. These reactions are often skin based or intestinal and in the general population are often described as the baby being a little intolerant to dairy. This is not true intolerance however. This is not a case where a food cannot be tolerated because the components needed to digest it are not present. This is, in fact, an allergy. The most common non-IgE symptoms manifest in 3 systems of the body: the Gastrointestinal System (e.g.stomach pain, cramps, diarrhea); the Respiratory System (e.g. Wheezing, coughing); the Skin (e.g eczema, hives). This has a different overall picture to lactose overload.

Allergy and Breastfeeding
Food components that we eat can pass into breastmilk, BUT it's not a simple picture. A 1984 study by Kilshaw & Cant looked at the passage of dairy and egg proteins into breastmilk. They looked at milk and blood from 29 women before and after they ate 1 raw egg and half a pint of cows milk. They found a cows milk protein (β-Lactuloglobuin) in the breastmilk of 10 out of 19 women who drank cows milk. They found an egg protein (ovalbumin) in the breastmilk of 13 out of 22 women who ate egg, and they found another egg protein (ovomucoid) in the breastmilk of 7 out of 9 women who ate egg. It was not found in the breastmilk of the other 8, 9 and 2 women respectively.
Essentially then, they found that foreign food proteins CAN pass in to breastmilk - but they don't consistently pass in all women, and that has to make us think a little. Breastmilk is made from our blood. The milk making cells (lactocytes) manufacture some of the components of breastmilk, but they are also very extensively supplied with blood vessels, and it is from the blood that many nutritional and immune components pass into the milk (proteins such as immunoglobulins, fats etc).
Lets go back one step further and look at mum's digestion. In my blog on reflux and stomach acid I discussed how proteins are supposed to be entirely broken down in to their constituent amino acids during digestion. The amino acids then pass through the gut wall into the bloodstream to be used in the body. Complete foreign proteins should not be in the bloodstream, yet studies like the one discussed above show that dairy and egg proteins can pass directly from our food into breastmilk completely unchanged in some women. So, why does this happen? Why in some and not in others?
The short answer is that we don't know. It may be that the mum actually has a leaky gut. It would take too long to go into leaky gut in this blog but I will link further articles in the further reading. Studies have shown that many food additives that we eat nowadays for example damage the tight junctions between cells in the gut wall and allow food particles through the gut walls. Perhaps the difference between the women in which the food passes and those in which it doesn't is their gut integrity. It may be that the mum is sensitised to some food proteins herself without realising - perhaps through her own feeding as an infant with formula or the way that solids were introduced. It may may that it is due to the type of food. Dairy and eggs (both of which are common allergens) are growth materials designed for the young of that species. They contain materials which are supposed to guide the growth of those young. Egg white provides the growth medium for a fetal chick as milk does for a mammal infant. In Baby Poop: What your paediatirican may not tell you, Linda Palmer says the following:
Animal milks have proteins that are quite similar to human milk proteins; they are similar but not identical. All milks are designed to buffer the digestive system - preserving the structure
of many of milk's proteins - and to allow certain milk proteins to pass right through a child's intestinal membrane....milk has valuable antibodies and other agents that are meant to pass into baby's bloodstream...If you think about it, egg-white is practically chicken milk
We know about the value of maternal antibodies to our babies and how our antibodies pass in milk and protect our babies, so here is the point that we need to confront what we are drinking when we drink the milk of another mammal. That milk is designed for her baby. Some proteins in that milk are designed to pass through the intestinal barrier.
Does that mean that we should all avoid dairy altogether? Again not a clear picture because a study looking at women with allergic family history who avoided dairy found them to have lower sIgA (secretory IgA) in their milk than the women who continued to eat dairy, and their babies had a higher incidence of cows milk allergy than the women who continued to eat dairy while breastfeeding (Jordan & Hogan, 2014). Secretory IgA is important for gut health and for gut integrity and in the early days babies cannot make it themselves. They only get it from breastmilk.
It's a complicated picture and the way that one mum and baby reacts to foods in their diet may be very different from the next. I've discussed the prevalence of allergies above but it's also important to note that not every fussy baby is reacting to something in your breastmilk. The first step for a fussy baby / fussy feeding / baby with suspected colic or reflux is a feeding assessment. The root causes I describe in my reflux blog are also appropriate here. Fussy, unhappy babies can be unhappy because of breastfeeding problems (poor milk transfer, oversupply, anxiety/stress in mum or baby, overstimulation, physical separation from caregiver, anatomical or functional restrictions), and breastfeeding problems have breastfeeding solutions. A thorough assessment and interventions to resolve these can allow a content, thriving baby to emerge. If other allergy symptoms sit along side the fussiness, (e.g. consistent projectile vomiting, consistently mucousy stools, excessive gas, constipation, blood in stools, eczema / skin rashes, persistent cradle cap, redness around the anus, chronic nasal stuffiness or mucus, frequent hiccups, repeated respiratory infections or colds etc) then it may be that the child is reacting to something in the diet. An IBCLC working through a breastfeeding assessment should also ask about and take account of these symptoms. It's important to note that of course allergies are not always food related. Skin rashes can be caused by reactions to creams, lotions, washing powders etc, and food allergies are not always the growth mediums of milk and eggs. Common food allergens are also nuts, wheat, soy, fish and shellfish.
Identifying what allergen your baby may be reacting to, and eliminating it can be another tricky area, and for another blog. A final word on eczema.... The prevalence of eczema and the acceptance of it as "normal" in babies really disturbs me. A study in England published in the Journal of the Royal Society of Medicine (Simpson 2009) found a increase of over 56% in prescriptions of eczema treatment over 2001-2005). They found that 1 in 9 people experience eczema at some stage in their life making it the most common chronic condition. Often when babies have eczema, creams are prescribed and parents reassured that they will simply grow out of the problem. As with everything, looking at the root cause of eczema is important I think. The skin is an organ. One of the primary functions of the skin is as a barrier between the inside of our bodies and the outside world. Another function is as an excretory organ. We excrete toxins and waste through the skin, primarily through sweat. Toxins in foods are eliminated through the liver and kidneys but if the liver and kidneys are perhaps congested with the amount they are dealing with, you get sluggish function (you often see constipation) then the body moves to other ways of excreting - often the skin or through the breath. In fact a 1995 study in the International Archives of Allergy & Immunology (Iukura et al, 1995) found that children with atopic eczema had reduced liver function. Complementary therapists and naturopaths often work on supporting the liver as well as looking at the gut in patients with skin rashes.
Eczema isn't a normal condition, and it isn't just cosmetic. It prevents normal function. It isn't normal for our protective barrier to break open. Children may indeed grow out of it later, but that doesn't mean it shouldn't be investigated now. I can't imagine anyone saying that a child would grow out of recurrent lesions appearing on any other organ.
In short if you are concerned about fussy behaviour in your baby and are worried about allergy - speak to an IBCLC or breastfeeding counsellor. Breastfeeding should be assessed first to look at root causes of the unhappiness in a baby, and as part of a thorough assessment allergy will be looked at. Blindly eliminating foods without assessment or any guidance can be stressful and confusing, and stress doesn't help when you are dealing with a crying baby. Reach out for breastfeeding help.
If you have any questions about a consultation or would like to arrange to meet, please get in touch.
Further Reading
1. Development of Lactase Persistence in Humans - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1182075/#!po=15.8537
2. UK Infant Feeding Survey - http://digital.nhs.uk/catalogue/PUB08694/Infant-Feeding-Survey-2010-Consolidated-Report.pdf
3. Prescribing Rates for Eczema - http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2746851/
4. Liver Function in Children with Eczema - http://www.karger.com/Article/Abstract/236973
5. Passage of Dietary Proteins in Breastmilk - http://www.karger.com/Article/Abstract/233582
6. Information on sIgA in Breastmilk - http://phenomena.nationalgeographic.com/2014/02/03/how-breast-milk-engineers-a-babys-gut-and-gut-microbes/
7. Reduction of sIgA in Breastmilk while on Elimination Diet - http://pediatrics.aappublications.org/content/134/Supplement_3/S139.1.full
8. Food additives causing change in intestinal permeability - http://www.sciencedirect.com/science/article/pii/S1568997215000245
9. Leaky Gut - https://chriskresser.com/9-steps-to-perfect-health-5-heal-your-gut/
Important Information
All material on this website is provided for educational purposes only. Online information cannot replace an in-person consultation with a qualified, independent International Board Certified Lactation Consultant (IBCLC) or your health care provider. If you are concerned about your health, or that of your child, consult with your health care provider regarding the advisability of any opinions or recommendations with respect to your individual situation.

